Shoulder Instability: Diagnosis and Treatment in Malleshwaram
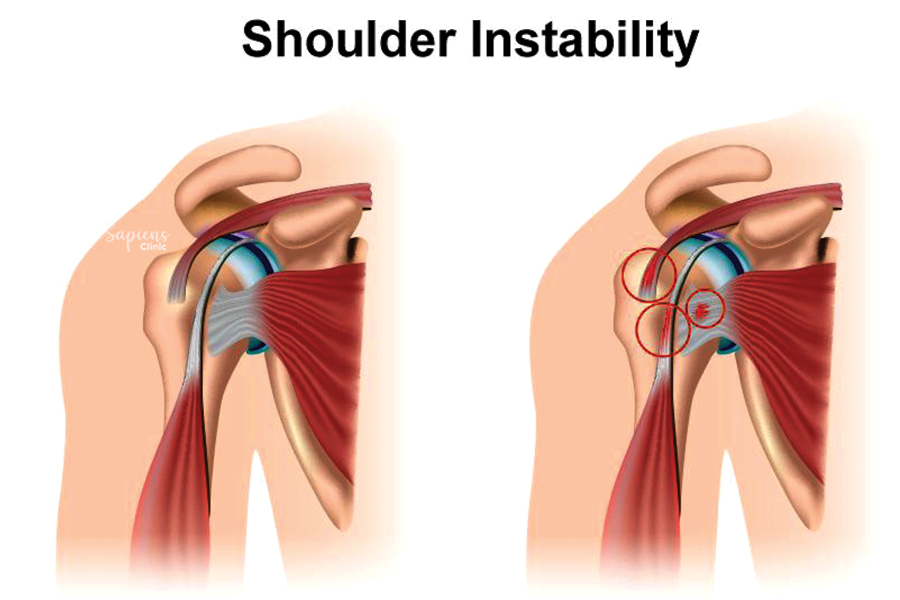
Shoulder instability occurs when the head of the upper arm bone (humerus) is forced out of the shoulder socket (glenoid), either partially (subluxation) or completely (dislocation). This condition can lead to pain, weakness and a sense of the shoulder “giving way.” At Sapiens Clinic in Malleshwaram, we specialize in diagnosing and treating shoulder instability, aiming to restore stability and function to the shoulder joint.
Understanding Shoulder Instability
The shoulder is the most mobile joint in the body, allowing a wide range of motion. However, this mobility makes it susceptible to instability. Shoulder instability can result from:
- Traumatic Injury: Such as a fall or collision causing the shoulder to dislocate.
- Repetitive Strain: Overuse from activities like swimming or throwing can stretch ligaments.
- Congenital Factors: Some individuals are born with naturally loose ligaments.
Instability can be classified as :
- Anterior: The most common, where the humerus slips forward.
- Posterior: Less common, with the humerus slipping backward.
- Multidirectional: Instability in multiple directions, often due to generalized ligament laxity.
Causes and Risk Factors
Factors contributing to shoulder instability include :
- Previous Dislocations: A history of shoulder dislocation increases the risk of recurrence.
- High-Risk Sports: Participation in contact or overhead sports like football or tennis.
- Connective Tissue Disorders: Conditions like Ehlers-Danlos syndrome can lead to ligament laxity.
Symptoms
Common symptoms of shoulder instability are :
- Pain: Especially during overhead activities.
- Weakness: A feeling of the shoulder being “dead” or lacking strength.
- Subluxation Sensation: A feeling that the shoulder is slipping out of place.
- Recurrent Dislocations: Multiple instances of the shoulder coming out of the socket.
Diagnosis
Diagnosing shoulder instability involves:
- Medical History: Discussing previous injuries and symptoms.
- Physical Examination: Assessing range of motion and joint stability.
- Imaging Tests: X-rays to detect bone damage; MRI to evaluate soft tissue injuries like labral tears.
Treatment Options
Non-Surgical Management
Initial treatment may include :
- Physical Therapy: Strengthening shoulder muscles to improve stability.
- Activity Modification: Avoiding movements that provoke instability.
- Medications: NSAIDs to reduce pain and inflammation.
Surgical Intervention
Surgery may be recommended for recurrent instability or when conservative treatments fail :
- Arthroscopic Bankart Repair: Reattaching the torn labrum to the glenoid.
- Latarjet Procedure: Transferring a piece of bone to the front of the glenoid to prevent dislocation.
- Capsular Shift: Tightening the joint capsule to reduce laxity.
The choice of procedure depends on the type and severity of instability, as well as patient-specific factors.
Recovery and Rehabilitation
Post-treatment rehabilitation focuses on :
- Immobilization: Using a sling to allow healing.
- Gradual Mobilization: Progressive exercises to restore range of motion.
- Strength Training: Building shoulder and scapular muscles to support the joint.
Recovery timelines vary, but most patients return to normal activities within 3 to 6 months.
Conclusion
Shoulder instability can significantly impact daily life and athletic performance. At Sapiens Clinic, Malleshwaram, Dr. Darshan Kumar A. Jain and our dedicated team provide comprehensive care, from accurate diagnosis to personalized treatment plans, ensuring optimal outcomes for our patients.
FAQs
1. Can shoulder instability heal without surgery?
Mild cases can improve with physical therapy and activity modification.
2. How do I know if I need surgery?
Surgery is considered if conservative treatments fail or if there are recurrent dislocations.
3. What is the success rate of shoulder instability surgery?
Surgical interventions like Bankart repair have high success rates, especially in young athletes.
4. Will I regain full shoulder function after treatment?
Most patients recover full function, especially with adherence to rehabilitation protocols.
5. How can I prevent shoulder instability?
Strengthening shoulder muscles and avoiding high-risk activities can reduce the risk.
Leave a Reply