Shoulder Dislocation: Diagnosis and Treatment in Malleshwaram
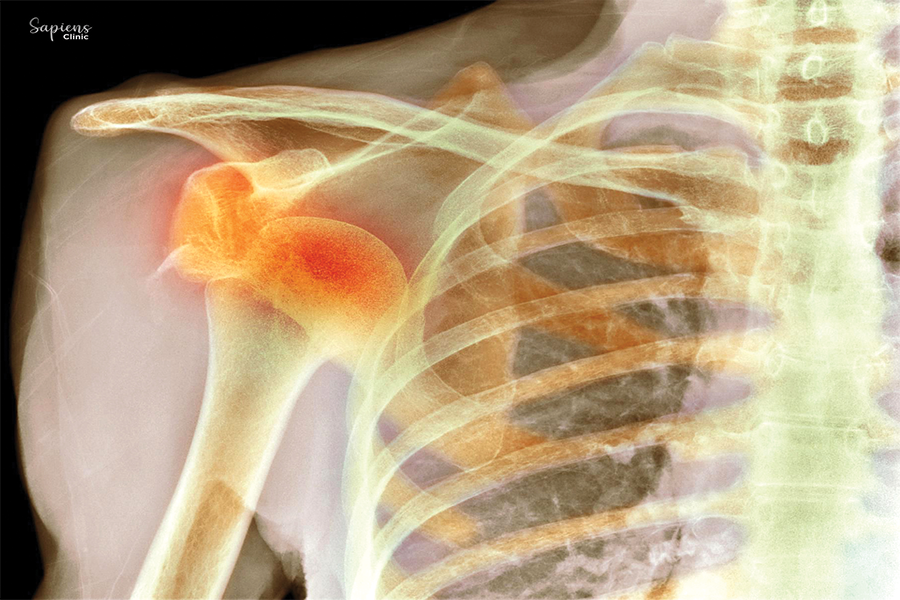
A shoulder dislocation occurs when the upper arm bone (humerus) is forced out of the cup-shaped socket (glenoid) of the shoulder blade. This injury can result in severe pain, instability, and limited mobility. At Sapiens Clinic in Malleshwaram, we specialize in the prompt diagnosis and effective treatment of shoulder dislocations, aiming to restore function and prevent recurrence.
Understanding Shoulder Dislocation
The shoulder is the body’s most mobile joint, making it susceptible to dislocations. Dislocations can be :
- Anterior: The most common type, where the humerus moves forward out of the socket.
- Posterior: Less common, often resulting from seizures or electric shocks.
- Inferior: Rare, typically caused by a sudden downward force.
Prompt medical attention is crucial to reposition the joint and prevent complications.
Causes and Risk Factors
Shoulder dislocations can result from :
- Trauma: Falls, sports injuries, or accidents.
- Overuse: Repetitive overhead motions weakening the joint.
- Congenital Conditions: Loose ligaments or shallow sockets.
Individuals engaged in contact sports or activities involving repetitive shoulder movements are at higher risk.
Symptoms
Common signs of a dislocated shoulder include :
- Severe Pain: Especially during movement.
- Visible Deformity: The shoulder may appear out of place.
- Swelling and Bruising: Around the joint.
- Limited Mobility: Difficulty moving the arm.
- Numbness or Tingling: In the arm or hand
Diagnosis
Accurate diagnosis involves:
- Physical Examination: Assessing the position and function of the shoulder.
- Imaging Tests: X-rays to confirm dislocation and check for fractures; MRI or CT scans for detailed views of soft tissues.
Treatment Options
Non-Surgical Management
Most shoulder dislocations can be treated without surgery :
- Closed Reduction: Gently maneuvering the bone back into place.
- Immobilization: Using a sling to keep the shoulder stable for a few weeks.
- Medication: Pain relievers and muscle relaxants to ease discomfort.
- Physical Therapy: Exercises to restore strength and range of motion.
Surgical Intervention
Surgery may be necessary for :
- Recurrent Dislocations: To tighten or repair torn ligaments.
- Severe Tissue Damage: Repairing or reconstructing damaged structures.
- Associated Fractures: Fixing broken bones around the shoulder.
Procedures like the Latarjet or Bankart repair are commonly performed to stabilize the joint.
Recovery and Rehabilitation
Recovery involves :
- Rest: Allowing tissues to heal.
- Gradual Exercise: Guided physical therapy to regain mobility.
- Avoiding High-Risk Activities: Until full recovery is achieved.
Full recovery can take several weeks to months, depending on the severity of the injury and adherence to rehabilitation protocols.
Conclusion
Shoulder dislocations, while common, require prompt and appropriate treatment to prevent long-term complications. At Sapiens Clinic, Malleshwaram, Dr. Darshan Kumar A. Jain and our dedicated team are committed to providing comprehensive care, from accurate diagnosis to personalized rehabilitation plans, ensuring optimal recovery and return to daily activities.
FAQs
1. Can a dislocated shoulder heal without treatment?
No, medical intervention is necessary to reposition the joint and prevent further damage.
2. How long does recovery take?
Recovery varies but typically ranges from a few weeks to several months, depending on the injury’s severity and treatment approach.
3. Is surgery always required for shoulder dislocations?
Not always. Many cases are managed non-surgically, but recurrent or severe dislocations may necessitate surgical intervention.
4. What are the risks of not treating a dislocated shoulder?
Untreated dislocations can lead to chronic instability, nerve damage, and increased risk of arthritis.
5. How can I prevent future dislocations?
Engaging in strengthening exercises, avoiding high-risk activities, and following medical advice can reduce the risk of recurrence.